Will it actually get better with time? Talking about dyspareunia, vaginismus and vulvodynia
"The pain will go away once you've had sex a few times. You'll get used to it. " Have you heard this before? Sex shouldn't hurt. Putting a tampon in shouldn't hurt. Yet, for some women they experience painful sex.
Because there are a few reasons why sex can be painful, I'm breaking down the difference between dyspareunia, vaginismus and vulvodynia.
Dyspareunia
Dyspareunia, the fancy word for painful sex, is essentially not a condition, per se, it's a symptom. It can happen with vaginismus or vulvodynia, but is not a condition like they are.
Painful sex can happen before, during, or after. It might be there when sex happens for the first time and every time after (primary dyspareunia) or it can happen after a period of painless sex (secondary dyspareunia).
When compared to vaginismus, women who experience dyspareunia have less sexual desire, lubrication, and penetration-related painful thoughts.
In terms of treatment, it's best to figure out the underlying reason of why the pain is happening.
Vaginismus
Do you ever feel like you're hitting a wall, or there's a sensation of no hole being down there? That might be because of vaginismus.
It's an involuntary muscle spasm of the pelvic floor (the set of muscles holding up your lower organs), incredibly tense pelvic floor muscles (it's like doing a bicep curl but never relaxing), impossibility of penetration, or fear of pain. The spasm can be felt at the opening of the vaginal canal.
Because it's a penetration disorder, you may experience pain with fingers, tampons, vaginal dilators, pap exams and sex. Although it happens with penetration, it's a physical AND an emotional disorder.
There are two types of vaginismus:
-
Situational vaginismus: sex might be a no-go, but inserting a tampon or finger doesn't hurt.
-
Spasmodic vaginismus: When the vagina spasms with penetration.
It's considered primary vaginismus when there has always been pain with sex, and secondary vaginismus when there has previously been painless sex.
Vaginismus may happen because of past sexual trauma, strict sexual or religious upbringing, fear of first-time sex (pain, bleeding, tearing, ripping, penis too large, vagina too small, sexually transmitted diseases, fear of pregnancy) or fear of pap exams.
Treatment usually involves a pelvic floor physiotherapy - dilators, biofeedback, and counseling with a sex therapist (which includes mindfulness, cognitive behavioural therapy and pyschotherapy).
Vulvodynia
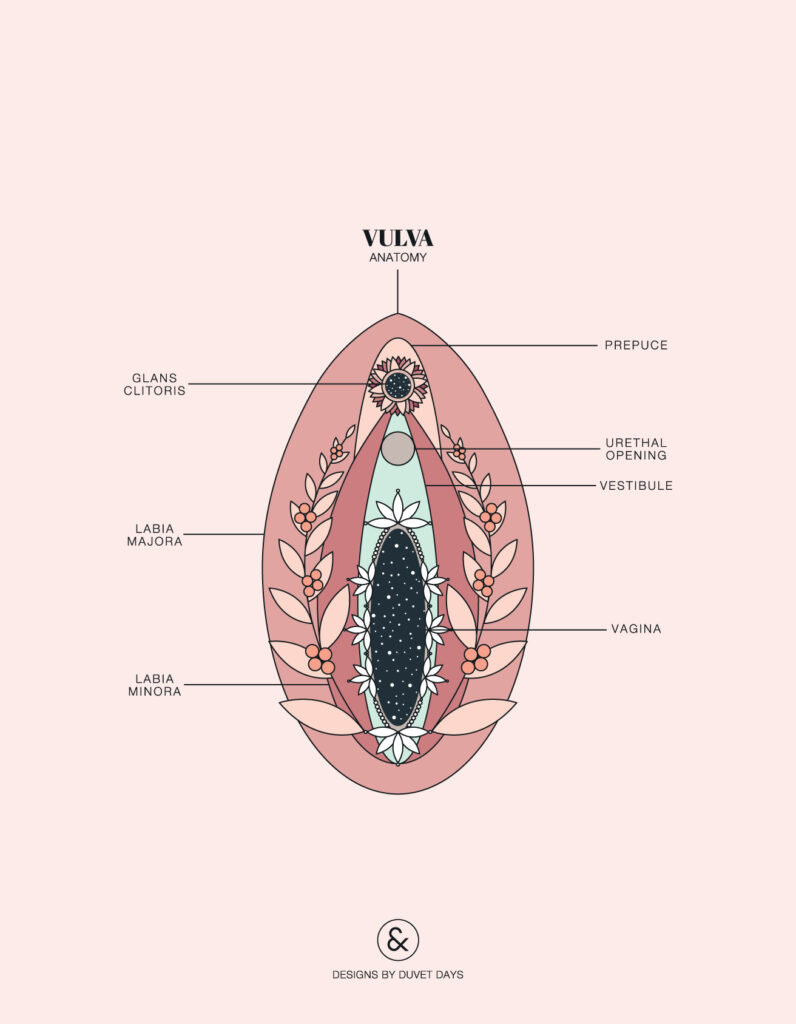
Vulvodynia (aka. vulvovestribular syndrome or vestibulodynia) is a chronic pain condition where there is vulvar inflammation and pain in the vulvar area.
There's no know cause of vulvodynia, so a bunch of conditions need to be ruled out before it's diagnosed. The pain also needs to be there for at least 3 months for it to be vulvodynia.
There are a couple types of vulvodynia:
-
Localized vulvodynia: pain in a distinct part of the vulva (ie. the vestibule)
-
Generalized vulvodynia: pain affecting the entire vulva
Pain can happen because:
-
Provoked vulvodynia: pain happens with touch (sexual or not sexual)
-
Unprovoked vulvodynia: pain happens without touch
Treatment usually involves a pelvic floor physiotherapist for muscle work, a sex therapist for counselling (like CBT), acupuncture with an acupuncturist or naturopathic doctor, or helping restore the vaginal microbiome, promoting healthy hormones and rebalancing the stress response with a naturopathic doctor.
Final Thoughts
Sex shouldn't be painful. And if it's something that you're experiencing, it's important to figure out why it's happening. Don't listen to people when they say "Can you just relax" or "Just tell yourself that sex won't hurt."
What you're feeling is real. Your experience is real. There are health professionals that can help you have pain-free sex. If you need any recommendations in the Toronto area, please let me know.
If you found this information helpful, please sign up for my monthly newsletter called The Flow for great and informative content like this!
References
Simonelli, C., Eleuteri, S., Petruccelli, F. and Rossi, R. (2014). Female sexual pain disorders. Current Opinion in Psychiatry, 27(6), pp.406-412.
Pacik, P. (2014). Understanding and treating vaginismus: a multimodal approach. International Urogynecology Journal, 25(12), pp.1613-1620.
